Knowledge Centre
Knowledge Centre
All
Insights
News
Articles
Videos
Search articles…

Health Communication
HealthTech
Patient Voice
Public & Global Health
Cliniphai and Gibson Research Consultancy Partner to Streamline Global COA and eCOA Translation Workflows
Featured
Health Communication
HealthTech
Patient Voice
The Nine Circles of Burden: Real-World Constraints on Patient Memory
Featured

Health Communication
Patient Voice
The Cognitive Burden Simulator: Complex Frequency Item on Distressing Mental Imagery
Health Communication
Patient Voice
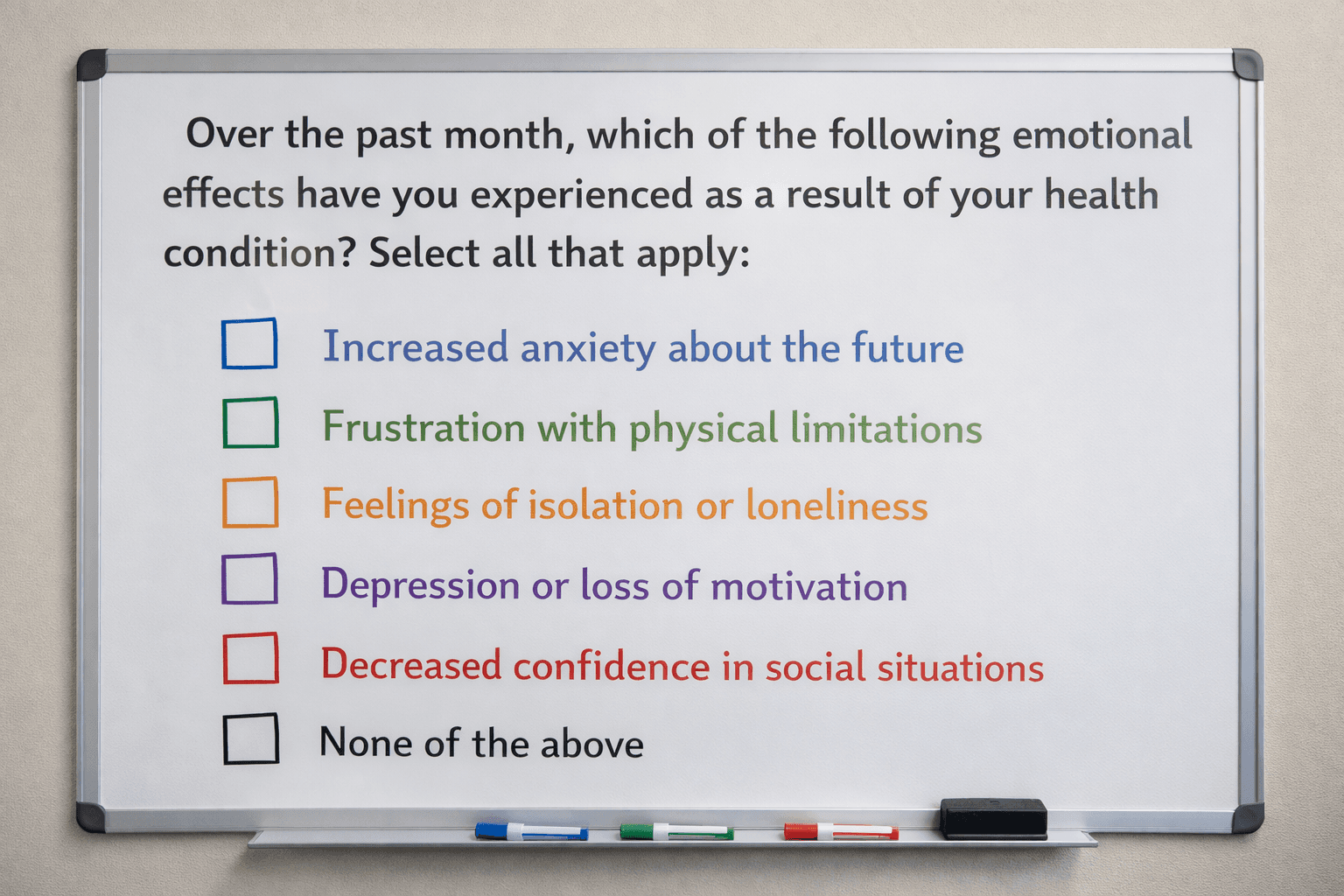
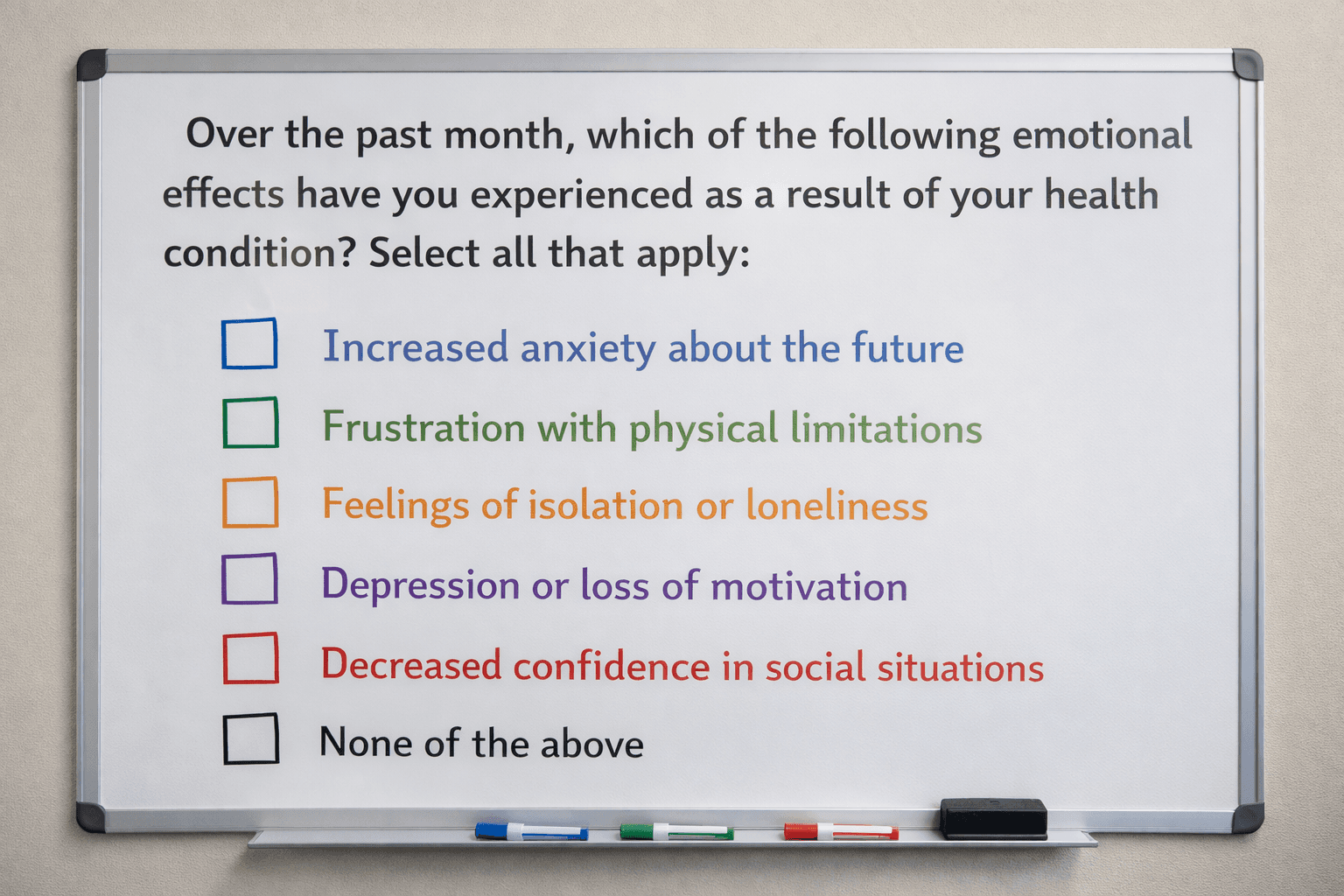
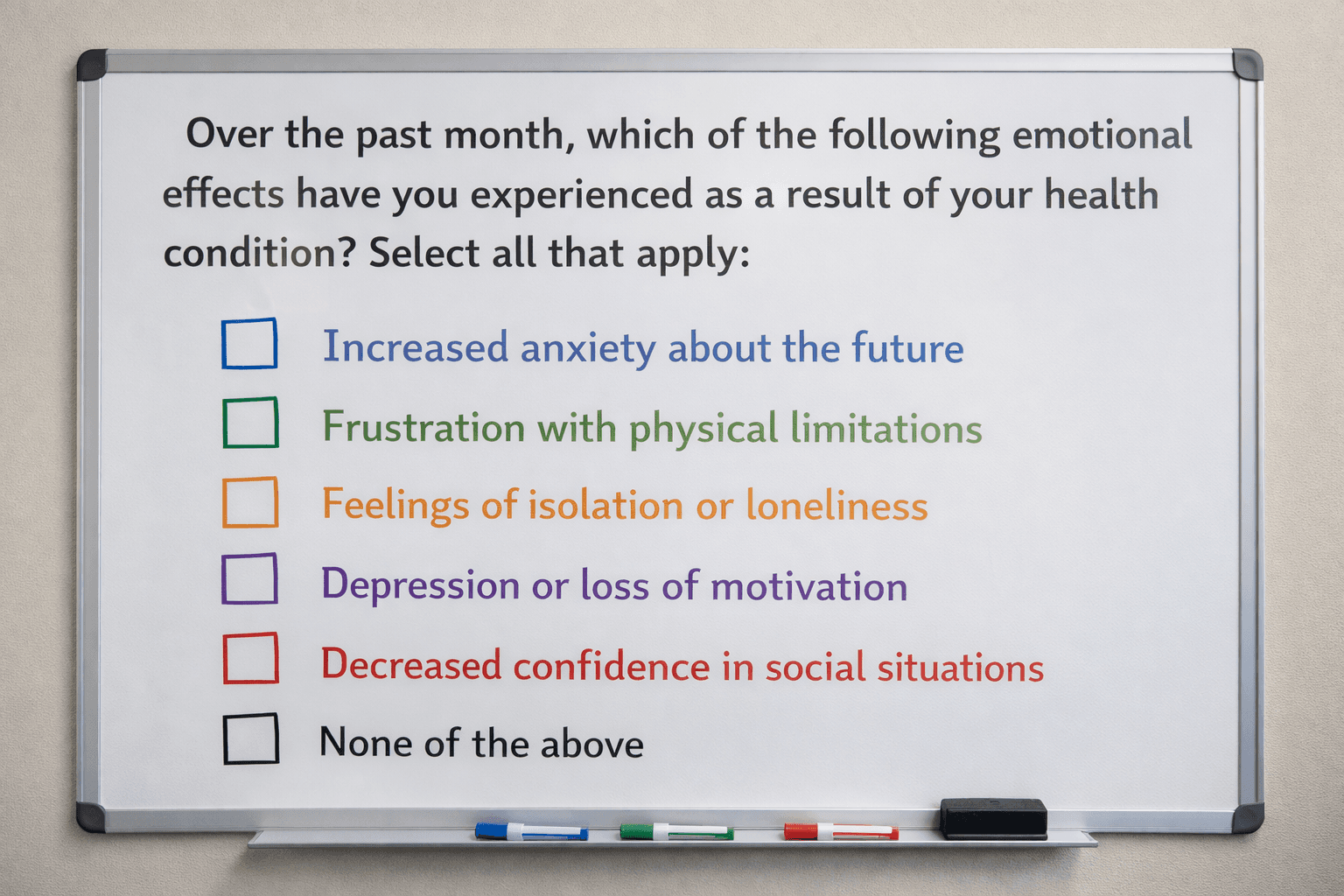
The Cognitive Burden Simulator: Checklist, Multi-Select PRO Items
Health Communication
Patient Voice
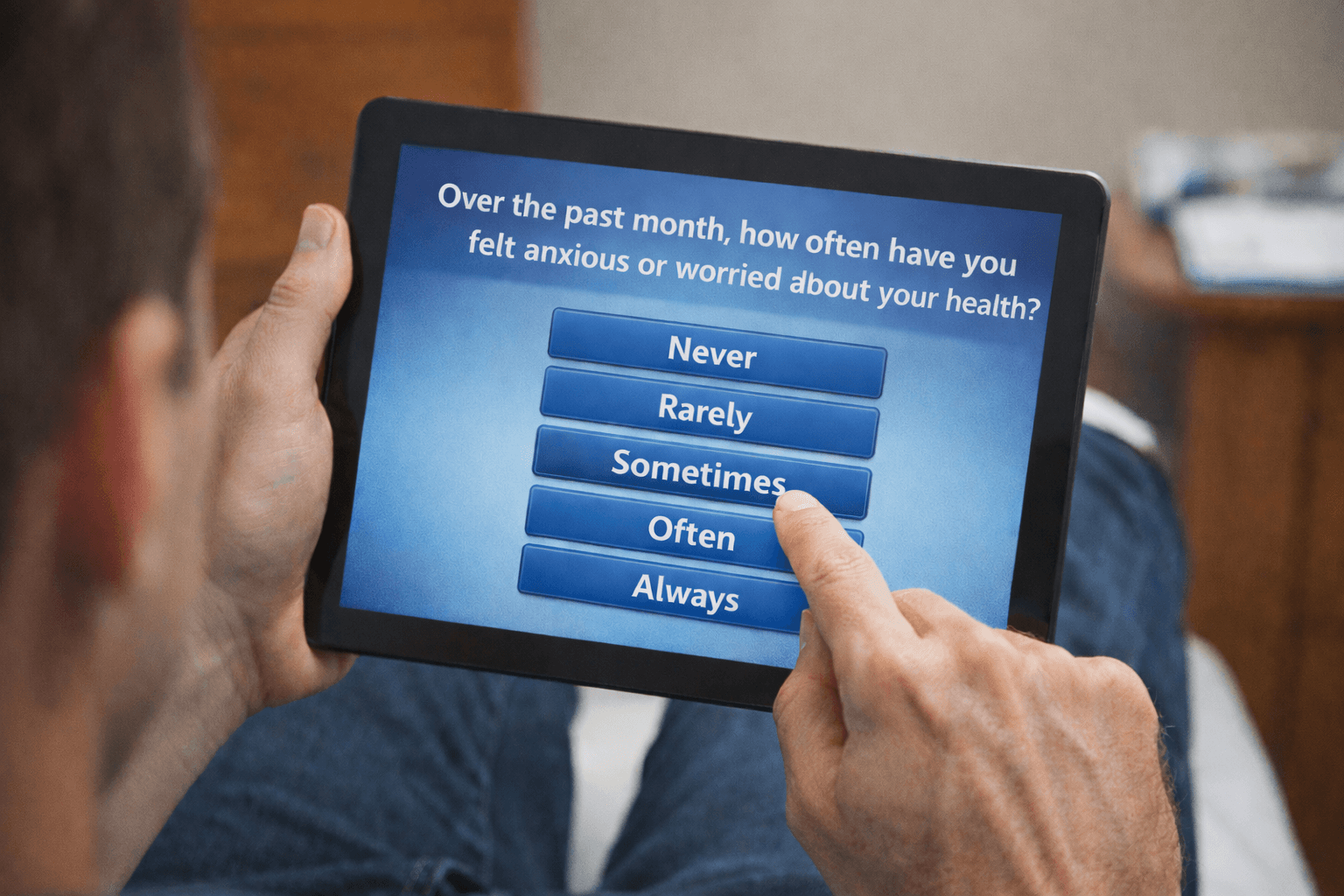
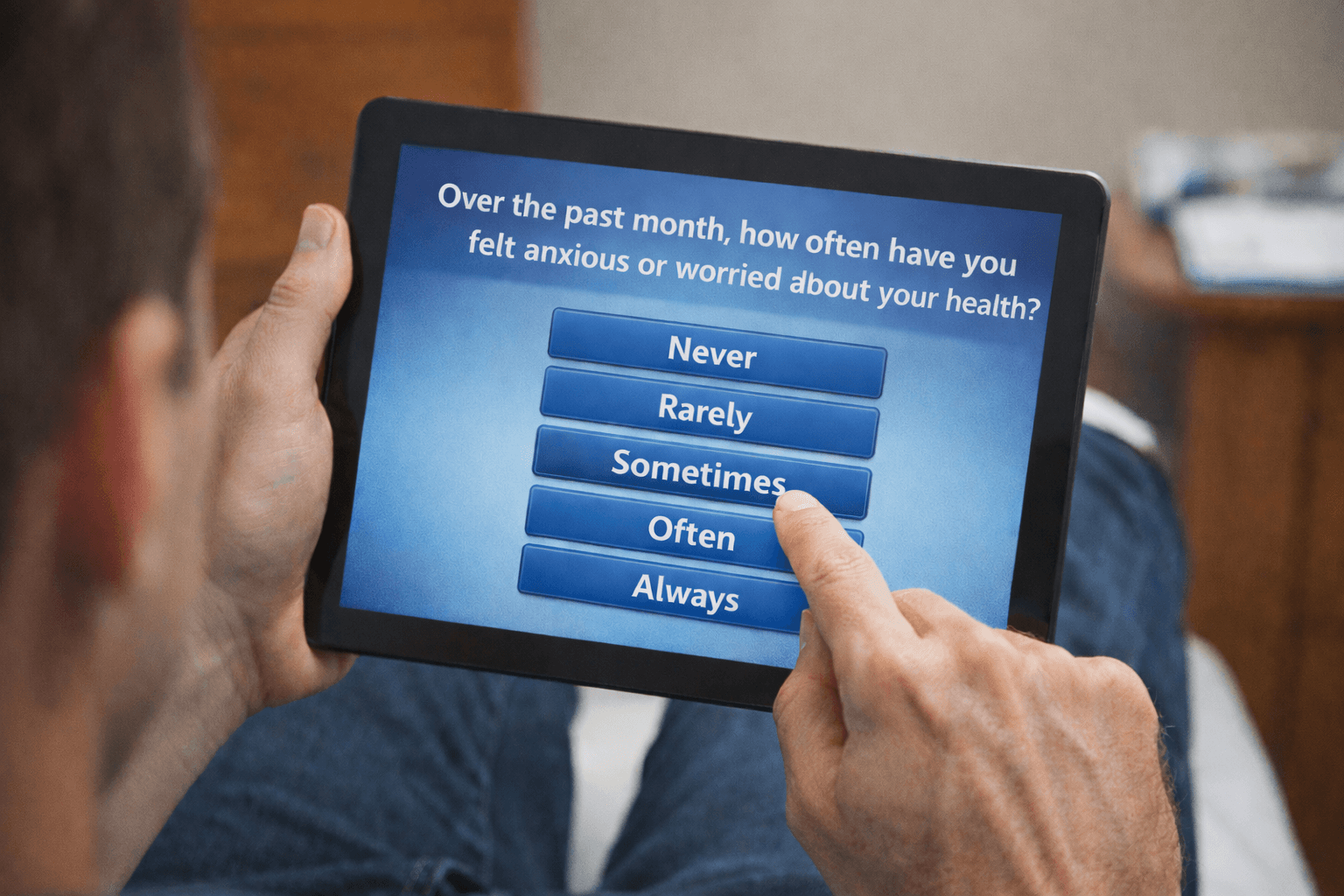
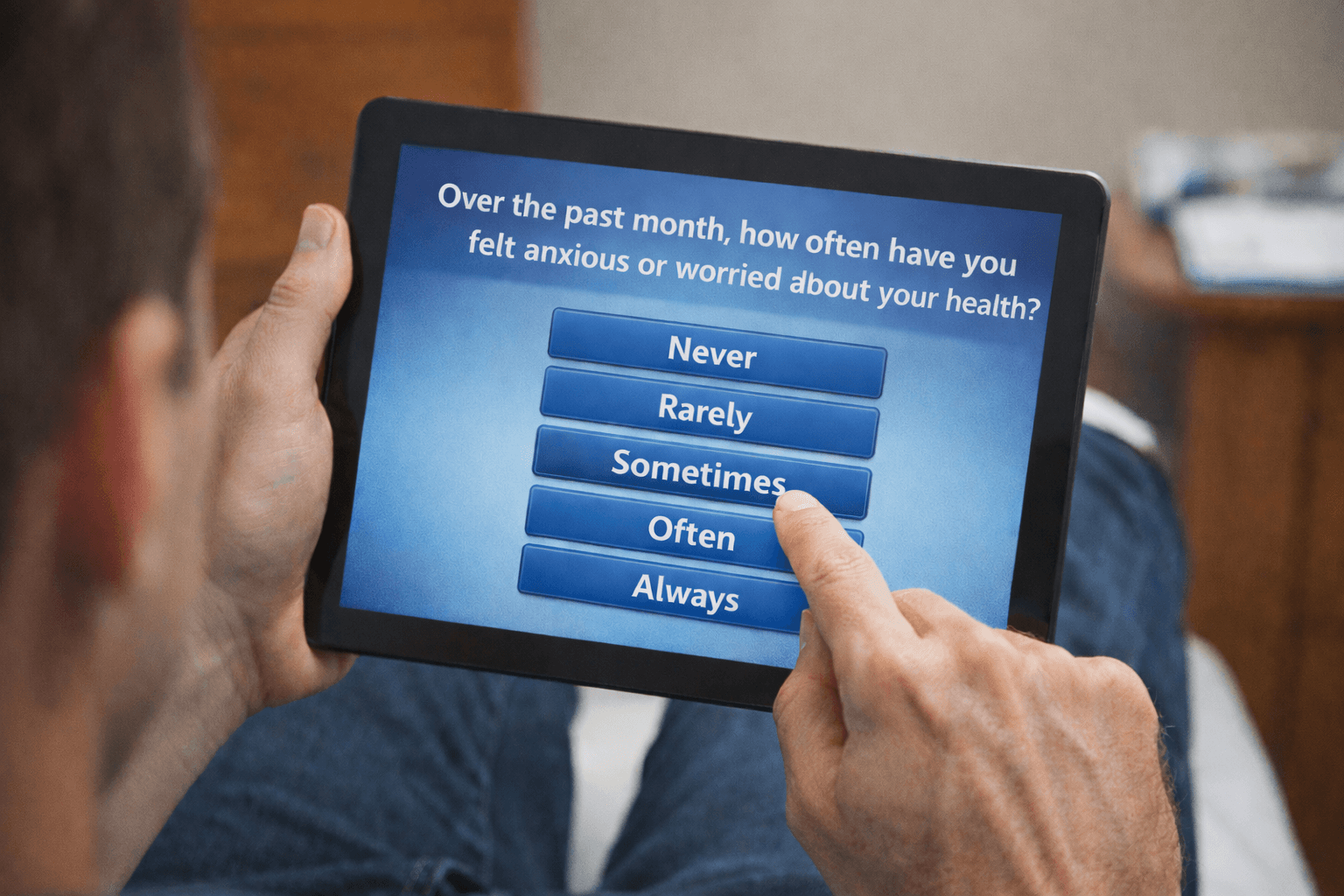
The Cognitive Burden Simulator: A Frequency Self-Report Item

Health Communication
Patient Voice
The Cognitive Burden Simulator: A Multi-Step Global Evaluation Item (With Follow-Up)

Health Communication
Patient Voice
The Cognitive Burden Simulator: The case of a COA Item with a Binary Response Choice

Health Communication
HealthTech
Patient Voice
From Google to ChatGPT: Offloading, Cognitive Debt and the Future of COAs

Health Communication
Patient Voice
Beyond the Magic: Baddeley’s Working Memory and Multi-Component Strain

Health Communication
Patient Voice
The Nine Circles of Burden: Mapping the Hidden Demands of COAs

Health Communication
Patient Voice
Working Memory and Clinical Outcome Assessments: A Comparative Load Analysis

Health Communication
Patient Voice
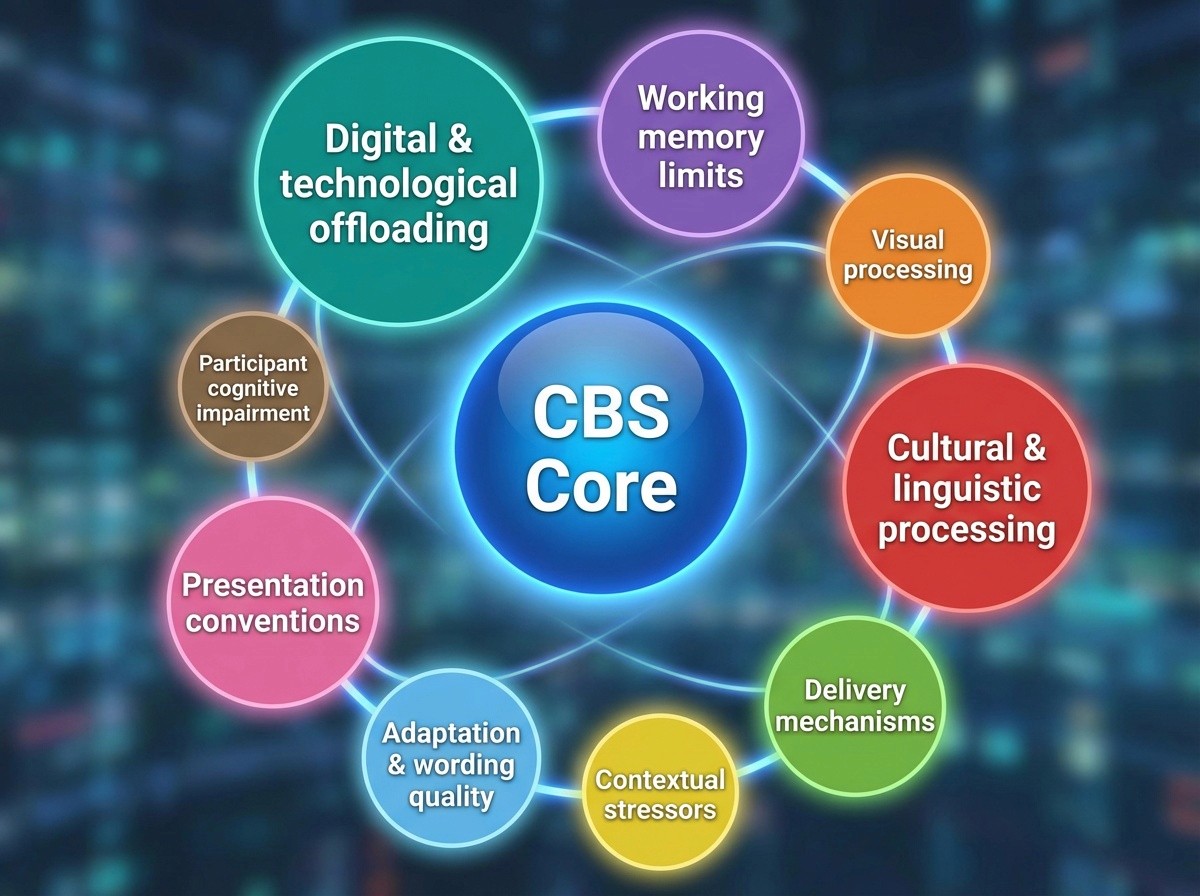
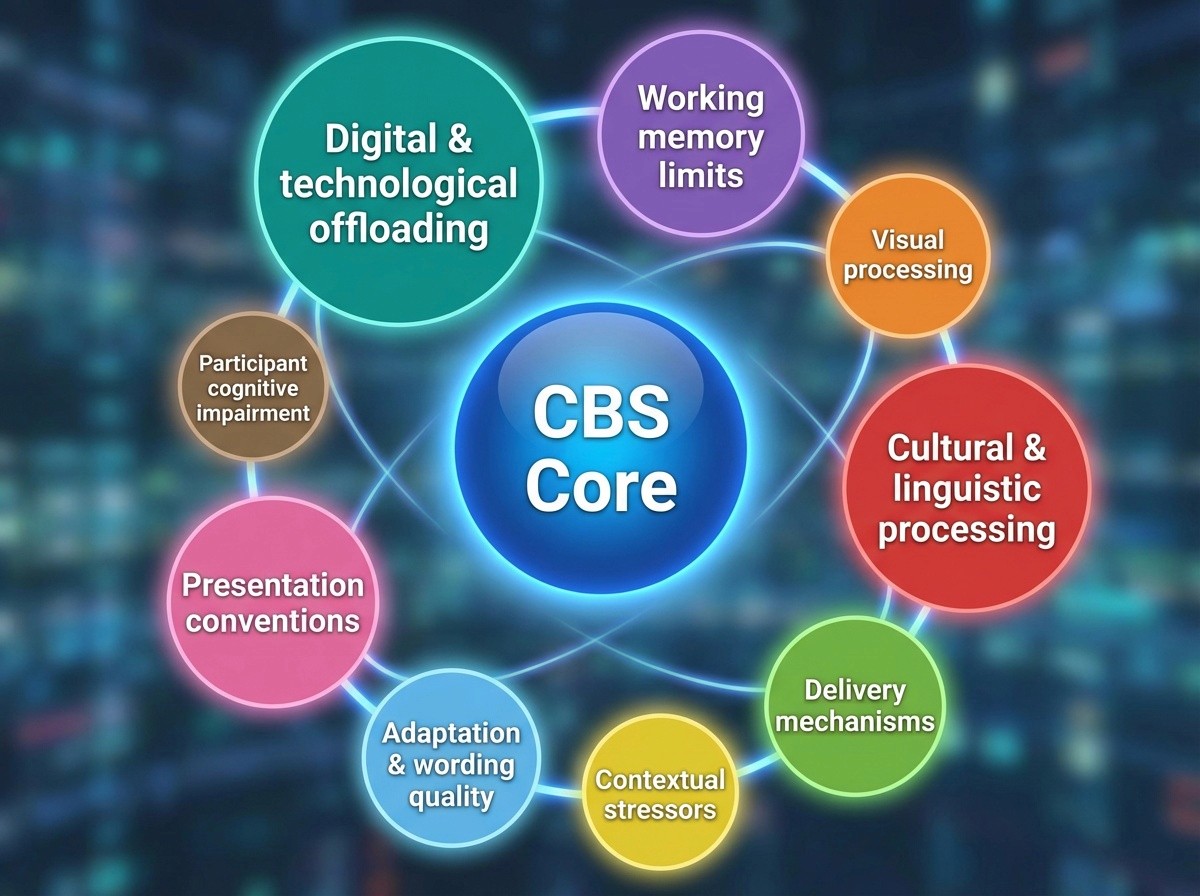
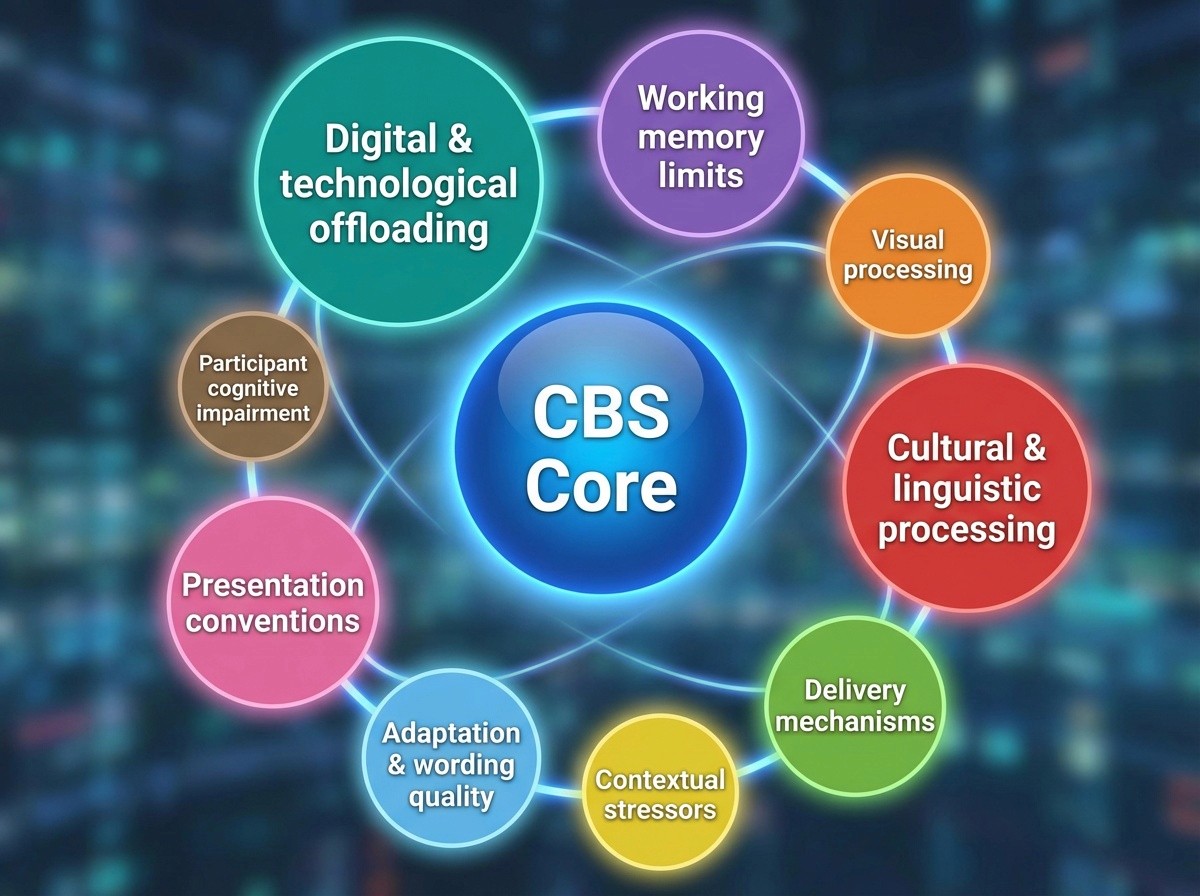
Background Behind the Cognitive Burden Simulator: Understanding the Hidden Demands of Clinical Outcome Assessments

Health Communication
Patient Voice
The Cognitive Burden Simulator: Visualising the Hidden Cognitive Burden of Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
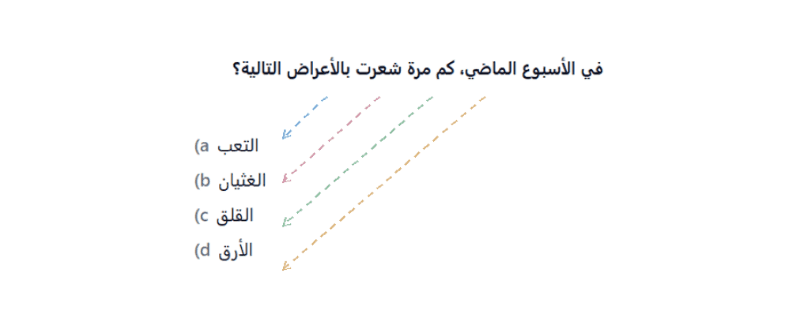
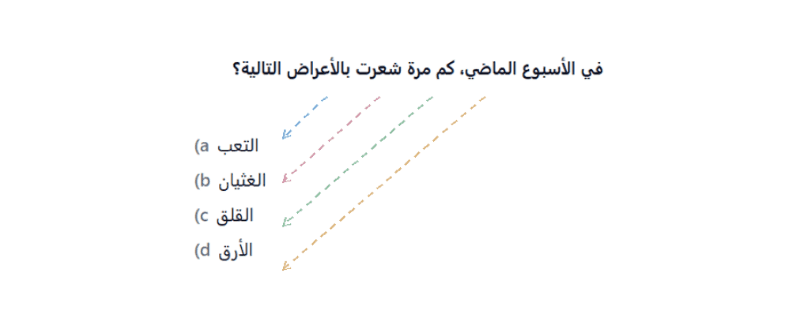
Cognitive Load and Non-Western Script Readers in Clinical Questionnaires: General Issues
Health Communication
Patient Voice
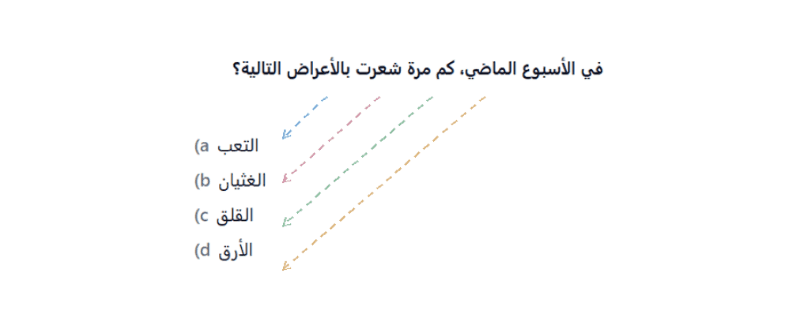
Cognitive Load and Shared-Stem Questions in Non-Western Script Contexts

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cognitive Load in Translation: Non-Western Patient Experiences with Western COAs

Health Communication
Health Promotion
Cognitive Load in Patient Communication: Patient Information Leaflets and Clinical Outcome Assessments Contrasted

Health Communication
Patient Voice
Reducing Cognitive Load in Clinical Outcome Assessments: Lessons from Mental Health, Pain Management and Oncology

Health Communication
Patient Voice
Cognitive Load in Clinical Outcome Assessments: Optimising Question Design for Better Data Quality
Health Communication
HealthTech
The Google Effect and Miller’s Magic Number: Implications for Questionnaire and Clinical Outcome Assessment Design.

Health Communication
Health Beliefs
Why the Presentation Often Stays the Same from Source to Target

Deep in the Shallow End: The emotional power of sacred trash that was never meant to last.

Health Communication
Patient Voice
The Field Beyond: Rumi, Reductionism and the Texture of Qualitative Knowing

The Conman Chronicles: Fictional Conversations between an AI Agent and a Wannabe New ‘Expert’

Health Communication
Patient Voice
Health Beliefs
Culture and Cognition in Survey Responses in Healthcare

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What I’ve Learnt About Using Visual Metaphors in Explainer Videos

Health Communication
Health Promotion
HealthTech
Public & Global Health
Designing Icons for Crisis, Emergency and Risk Communication

Health Communication
Why Visual Clarity Can Save Lives: Designing for thinking under stress.

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Empowered Patient: A Privileged Identity?

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cross-Cultural Aspects of the Locus of Control

Patient Voice
Health Beliefs
When Control Lies Beyond: The External Locus of Control in Healthcare and Life

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Power Within: Internal Locus of Control as a Core of Patient Empowerment

Health Communication
Patient Voice
Owning the Outcome: Understanding the Internal Locus of Control in Health and Beyond

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
When the Sublime Offends: Ethical Collisions and Cultural Limits

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Ambiguous States, Ambivalent Roles: Liminality in the Clinical Encounter

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Beyond Beauty: Reclaiming the Sublime in Culture and Care

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Biographical Disruption and the Liminal Self

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Threshold of Meaning: The Liminality of Culture in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Measuring What Matters: How Do You Capture Resonance in Health Communication?

Patient Voice
Public & Global Health
Exploring Research Design: The Grand Heist’s Blueprint

Health Communication
Patient Voice
Public & Global Health
Why Does Informed Consent Matter?

Health Communication
Patient Voice
Public & Global Health
5 Tips for Achieving Truly Informed Consent in Research

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Messaging and Culture: Reaching What Lies Beneath

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion Campaigns Fall Flat When They Ignore the Depths

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Charting the Unseen: What COAs Miss Beneath the Cultural Waterline

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Every Individual is a Culture of One. Responding to the Sublime in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Sublime: Culture’s Deep and Unseen Role in Shaping Health Behaviours

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Culture is Never a Frozen List of Traits

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
What Linguistic Relativity Really Looks Like. How language shapes attention, memory and perception across cultures

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 2: Time to Let it Melt

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 1: Language, Culture and Conceptual Equivalence in Translation

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion and Health Beliefs

Health Communication
HealthTech
Patient Voice
Public & Global Health
The Vice of Time and Cost

HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Dragonfly Trapped in Amber: When Method Becomes Dogma

Health Communication
Patient Voice
Public & Global Health
Linguistic Validation Specialisation Course

Health Communication
HealthTech
The Predictable Rhetoric of AI-Generated Text: Overused Stylistic Devices

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
"Sí da / No da": Calm Public Health Messaging That Worked

Health Communication
Health Promotion
Public & Global Health
How Smart Public Health Campaigns Avoid the Irony Trap

Health Communication
Health Promotion
Public & Global Health
The Irony Trap: How public health messages get hijacked by culture

Patient Voice
Public & Global Health
Health Beliefs
Gynecology in Turkey: Navigating Cultural and Social Taboos

Health Communication
Public & Global Health
Health Beliefs
Addressing Mental Health Stigma in Turkey

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Experiments in Language: AI as a Co-Creator in Global Health Communication

Health Communication
HealthTech
Rethinking Work: The Personal and Professional Shift with AI

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Semiotics of the White Coat in Media Communication

Health Communication
Health Promotion
Public & Global Health
Epilogue: The Tylenol-Autism Debate, the Knowledge Gap and the Future of Trust

Health Communication
Health Promotion
Public & Global Health
“Tough It Out”: The Long Dismissal of Women’s Pain

Health Communication
Health Promotion
Public & Global Health
The “Tough It Out” Line: Why It Resonated, Why It Harms

Health Communication
Health Promotion
HealthTech
Public & Global Health
Why Falsehoods Travel Faster: The Facts versus Emotion Gap

Health Communication
Health Promotion
Public & Global Health
Speaking in Facts, Hearing in Feelings

Health Communication
Health Promotion
Public & Global Health
The Tylenol-Autism Controversy: Communication, Power and the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Did We Bend Technology Out of Shape? From the Handaxe to the Health App

Health Communication
HealthTech
What’s That Coming Over the Hill? How We Use AI In Our Work

Health Communication
HealthTech
Public & Global Health
Bridging Concept Elaboration and Translatability in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Translatability in Clinical Outcome Assessments: Designing for the Global Patient Voice

Health Communication
Patient Voice
Health Beliefs
Concept Elaboration in Clinical Outcome Assessments: An intersection of Language, Science and Culture

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Do Not Ignore Visuals When Testing Materials

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Designing Beyond Obsolescence

Health Communication
Health Promotion
HealthTech
Public & Global Health
The Lifecycle of Visual Symbols

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Dead Metaphors and Digital Assumptions

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What is Really Intuitive? Mapping the Learnability of Visuals

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Illusion of Intuition: Why “Obvious” Visuals Are Not Always Obvious

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not All Visuals Are Instantly Understood

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Choosing the Right Visuals Across Healthcare Communication

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Rise of Visual Communication in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Flexible Visuals within a Fixed Logic

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not Everyone Reads the Same Picture in the Same Way

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Designing Visuals That Teach And Not Just Tell

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Seeing is not Understanding: Visual Literacy and Why It Matters in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Are Icons Really Universal? Rethinking Visual Language in Global Healthcare

Health Communication
HealthTech
Health Beliefs
From Text to Visual: How Reading Behaviour is Changing in the Digital Age

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Pushing the Round Peg of Typography Through the Square Hole of Culture

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Script Complexity, Typography and COA Design

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: The Hidden Impact of Layout Mismatches on Reading Efficiency

Health Communication
Health Promotion
Patient Voice
Public & Global Health
The Anatomy of Reading: Rethinking Logo Placement in Patient-Facing Materials

Health Communication
Public & Global Health
How Culture Shapes the Way We Read Clinical and Technical Documents

HealthTech
Patient Voice
Health Beliefs
As the Ox Turns: The Biological, Cultural and Technological Limits of Reading

Health Communication
Health Promotion
When Cultural Differences in Information Processing and Typography Create Barriers in COA Localisation

Health Communication
Patient Voice
Linguistic Validation of Clinical Outcome Assessments (COAs): A Checkbox Activity or an Opportunity for Research?

Health Communication
HealthTech
Patient Voice
What does Cognitive Debriefing NOT Cover in a Clinical Outcome Assessment?

Health Communication
Patient Voice
Response Biases and Cognitive Differences in the Cross-Cultural Use of Clinical Outcomes Assessments

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Cultural and Contextual Considerations in the COA Localisation Process

Health Communication
Public & Global Health
Audience Design in Health Communication: Tailoring the Message for Effective Engagement

Health Communication
HealthTech
Formality and Politeness in Clinical Outcome Assessments (COAs) – A Sociolinguistic Perspective on Audience Design

Health Communication
Health Promotion
Patient Voice
Cultural Coating in COA Translation: Overcoming Linguistic and Semantic Barriers

Health Communication
Health Promotion
Health Beliefs
Common Problems of Localisation in Clinical Outcome Assessments (COAs)

Health Communication
Not the Yellow from the Egg: Using Figurative Language in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Taboo Topics in Health: How These Can Lead to ‘Cultural Coating’ of Items in COA Development

Health Communication
Addressing Lexical Ambiguities in Clinical Outcome Assessments: Design with the Entire World in Mind

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Eight tips for Best Practice in Questionnaire Design in Clinical Outcome Assessments

Health Communication
Patient Voice
Public & Global Health
Clinical Outcome Assessments: investing millions only to get the basics wrong?

Health Communication
Patient Voice
Health Beliefs
Assent: Information Overload and Cultural Communication Styles

Health Communication
Patient Voice
Redesigning Assent Forms in International Clinical Research

Health Communication
Patient Voice
A Critique of Clinical Trial Informed Consent and Patient Information Sheets in Clinical Trials

Health Communication
Health Promotion
Patient Voice
Public & Global Health
A Comparison of Formative versus Summative Readability Testing

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Readability User Testing: Strengths, Weaknesses and Strategic Approaches for Patient Information Leaflets

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Essential Tips for Creating IFUs That People Actually Read

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Do not do these 10 mistakes when designing Risk Minimisation Patient Cards

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Clear as Mud: The Hidden Complexity of Simple Drug Instructions

Health Communication
Public & Global Health
Not So Simple: The Hidden Complexity of Everyday Drug Instructions

Health Communication
Public & Global Health
Health Beliefs
Lost in Translation: The Hidden Confusion Behind Simple Medicine Instructions

Health Communication
HealthTech
Public & Global Health
The Opportunities and Challenges of Electronic Patient Information Leaflets (ePILs)

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Knowledge Gap Is Still a Choice

Health Communication
Public & Global Health
Common Design Shortcomings in Written Patient Information

Health Communication
Public & Global Health
Patient Engagement in the form of Patient Information Leaflets. Has the needle even moved since the 2000s?

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Consequences of the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Narrowing the Knowledge Gap between the Pharmaceutical Industry and Their Consumers

Health Communication
Patient Voice
Bridging the Knowledge Gap in Patient Communication in the Provider-Patient Relationship

Health Communication
HealthTech
Patient Voice
Health Beliefs
The Impact of the Knowledge Gap on Patient Well-being

Health Communication
Patient Voice
Face-Sensitive Patient Documentation Across Cultures: Can One Size Fit All?

Health Communication
Patient Voice
Health Beliefs
Face-Sensitive Communication in Pharma: Cultural Impacts on Patient Engagement

Health Communication
HealthTech
Patient Voice
Considerations of ‘Face-Sensitivity’ when Planning Patient-Facing Documentation

Health Communication
Patient Voice
The Blind Spot of Pharma: Information Design as an ‘Unknown Unknown’

Health Communication
Patient Voice
Face Maintenance and Patient Voice in Patient Engagement: The Ideal versus Reality

Health Communication
Patient Voice
Beyond Words: How Face Maintenance Shapes Patient Communication and Engagement

Health Communication
Patient Voice
Can the Pragmatics of Face Maintenance be Mapped onto Patient Engagement Practices?

Patient Voice
Public & Global Health
Health Beliefs
Global Perspectives on Patient Engagement in Clinical Settings

HealthTech
Patient Voice
Patient Engagement in Clinical Practice: what are the key differences between the UK and the USA?

Patient Voice
Health Beliefs
The Cultural Dimensions of Patient Engagement: Challenges for the Pharmaceutical Industry

Health Communication
Patient Voice
Why is Tokenism Rife in the Adoption of Patient Voice Activities?

Health Promotion
Patient Voice
Public & Global Health
The Knowledge Gap between the Medical Establishment and the Patient is a Choice

Patient Voice
Health Beliefs
This Far but No Further: the Cruel Fiction of Patient Empowerment

Health Communication
HealthTech
Patient Voice
The ‘Service Refugee’ Companies Chasing Patient Voice Research: What They Should Know

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Sliding Scale of Sincerity towards the Patient Voice Agenda

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
In Spite of Our Business Model

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Linking Up the Silos

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
A Belated Introduction to Gibson Research Consultancy (GRC)

Patient Voice
Health Beliefs
Challenges of Integrating Patient Voice into Clinical Research in Turkey

Patient Voice
Avoiding Tokenism: Strategies for Meaningful Involvement in Patient and Public Involvement (PPI) Research

Patient Voice
Why Does Tokenistic Patient and Public Involvement (PPI) in Research Occur?

Patient Voice
Understanding Lived Experience Research: A Person-Centred Approach to Knowledge

Patient Voice
The History of Lived Experience Research and Patient and Public Involvement

Patient Voice
Becoming a Lived Experience Researcher – Or, in Layman’s Terms, Putting the Psycho in Psychology
All
Insights
News
Articles
Videos
Search articles…

Health Communication
HealthTech
Patient Voice
Public & Global Health
Cliniphai and Gibson Research Consultancy Partner to Streamline Global COA and eCOA Translation Workflows
Health Communication
HealthTech
Patient Voice
The Nine Circles of Burden: Real-World Constraints on Patient Memory

Health Communication
Patient Voice
The Cognitive Burden Simulator: Complex Frequency Item on Distressing Mental Imagery
Health Communication
Patient Voice
The Cognitive Burden Simulator: Checklist, Multi-Select PRO Items
Health Communication
Patient Voice
The Cognitive Burden Simulator: A Frequency Self-Report Item

Health Communication
Patient Voice
The Cognitive Burden Simulator: A Multi-Step Global Evaluation Item (With Follow-Up)

Health Communication
Patient Voice
The Cognitive Burden Simulator: The case of a COA Item with a Binary Response Choice

Health Communication
HealthTech
Patient Voice
From Google to ChatGPT: Offloading, Cognitive Debt and the Future of COAs

Health Communication
Patient Voice
Beyond the Magic: Baddeley’s Working Memory and Multi-Component Strain

Health Communication
Patient Voice
The Nine Circles of Burden: Mapping the Hidden Demands of COAs

Health Communication
Patient Voice
Working Memory and Clinical Outcome Assessments: A Comparative Load Analysis

Health Communication
Patient Voice
Background Behind the Cognitive Burden Simulator: Understanding the Hidden Demands of Clinical Outcome Assessments

Health Communication
Patient Voice
The Cognitive Burden Simulator: Visualising the Hidden Cognitive Burden of Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Cognitive Load and Non-Western Script Readers in Clinical Questionnaires: General Issues
Health Communication
Patient Voice
Cognitive Load and Shared-Stem Questions in Non-Western Script Contexts

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cognitive Load in Translation: Non-Western Patient Experiences with Western COAs

Health Communication
Health Promotion
Cognitive Load in Patient Communication: Patient Information Leaflets and Clinical Outcome Assessments Contrasted

Health Communication
Patient Voice
Reducing Cognitive Load in Clinical Outcome Assessments: Lessons from Mental Health, Pain Management and Oncology

Health Communication
Patient Voice
Cognitive Load in Clinical Outcome Assessments: Optimising Question Design for Better Data Quality
Health Communication
HealthTech
The Google Effect and Miller’s Magic Number: Implications for Questionnaire and Clinical Outcome Assessment Design.

Health Communication
Health Beliefs
Why the Presentation Often Stays the Same from Source to Target

Deep in the Shallow End: The emotional power of sacred trash that was never meant to last.

Health Communication
Patient Voice
The Field Beyond: Rumi, Reductionism and the Texture of Qualitative Knowing

The Conman Chronicles: Fictional Conversations between an AI Agent and a Wannabe New ‘Expert’

Health Communication
Patient Voice
Health Beliefs
Culture and Cognition in Survey Responses in Healthcare

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What I’ve Learnt About Using Visual Metaphors in Explainer Videos

Health Communication
Health Promotion
HealthTech
Public & Global Health
Designing Icons for Crisis, Emergency and Risk Communication

Health Communication
Why Visual Clarity Can Save Lives: Designing for thinking under stress.

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Empowered Patient: A Privileged Identity?

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cross-Cultural Aspects of the Locus of Control

Patient Voice
Health Beliefs
When Control Lies Beyond: The External Locus of Control in Healthcare and Life

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Power Within: Internal Locus of Control as a Core of Patient Empowerment

Health Communication
Patient Voice
Owning the Outcome: Understanding the Internal Locus of Control in Health and Beyond

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
When the Sublime Offends: Ethical Collisions and Cultural Limits

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Ambiguous States, Ambivalent Roles: Liminality in the Clinical Encounter

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Beyond Beauty: Reclaiming the Sublime in Culture and Care

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Biographical Disruption and the Liminal Self

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Threshold of Meaning: The Liminality of Culture in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Measuring What Matters: How Do You Capture Resonance in Health Communication?

Patient Voice
Public & Global Health
Exploring Research Design: The Grand Heist’s Blueprint

Health Communication
Patient Voice
Public & Global Health
Why Does Informed Consent Matter?

Health Communication
Patient Voice
Public & Global Health
5 Tips for Achieving Truly Informed Consent in Research

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Messaging and Culture: Reaching What Lies Beneath

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion Campaigns Fall Flat When They Ignore the Depths

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Charting the Unseen: What COAs Miss Beneath the Cultural Waterline

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Every Individual is a Culture of One. Responding to the Sublime in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Sublime: Culture’s Deep and Unseen Role in Shaping Health Behaviours

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Culture is Never a Frozen List of Traits

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
What Linguistic Relativity Really Looks Like. How language shapes attention, memory and perception across cultures

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 2: Time to Let it Melt

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 1: Language, Culture and Conceptual Equivalence in Translation

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion and Health Beliefs

Health Communication
HealthTech
Patient Voice
Public & Global Health
The Vice of Time and Cost

HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Dragonfly Trapped in Amber: When Method Becomes Dogma

Health Communication
Patient Voice
Public & Global Health
Linguistic Validation Specialisation Course

Health Communication
HealthTech
The Predictable Rhetoric of AI-Generated Text: Overused Stylistic Devices

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
"Sí da / No da": Calm Public Health Messaging That Worked

Health Communication
Health Promotion
Public & Global Health
How Smart Public Health Campaigns Avoid the Irony Trap

Health Communication
Health Promotion
Public & Global Health
The Irony Trap: How public health messages get hijacked by culture

Patient Voice
Public & Global Health
Health Beliefs
Gynecology in Turkey: Navigating Cultural and Social Taboos

Health Communication
Public & Global Health
Health Beliefs
Addressing Mental Health Stigma in Turkey

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Experiments in Language: AI as a Co-Creator in Global Health Communication

Health Communication
HealthTech
Rethinking Work: The Personal and Professional Shift with AI

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Semiotics of the White Coat in Media Communication

Health Communication
Health Promotion
Public & Global Health
Epilogue: The Tylenol-Autism Debate, the Knowledge Gap and the Future of Trust

Health Communication
Health Promotion
Public & Global Health
“Tough It Out”: The Long Dismissal of Women’s Pain

Health Communication
Health Promotion
Public & Global Health
The “Tough It Out” Line: Why It Resonated, Why It Harms

Health Communication
Health Promotion
HealthTech
Public & Global Health
Why Falsehoods Travel Faster: The Facts versus Emotion Gap

Health Communication
Health Promotion
Public & Global Health
Speaking in Facts, Hearing in Feelings

Health Communication
Health Promotion
Public & Global Health
The Tylenol-Autism Controversy: Communication, Power and the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Did We Bend Technology Out of Shape? From the Handaxe to the Health App

Health Communication
HealthTech
What’s That Coming Over the Hill? How We Use AI In Our Work

Health Communication
HealthTech
Public & Global Health
Bridging Concept Elaboration and Translatability in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Translatability in Clinical Outcome Assessments: Designing for the Global Patient Voice

Health Communication
Patient Voice
Health Beliefs
Concept Elaboration in Clinical Outcome Assessments: An intersection of Language, Science and Culture

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Do Not Ignore Visuals When Testing Materials

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Designing Beyond Obsolescence

Health Communication
Health Promotion
HealthTech
Public & Global Health
The Lifecycle of Visual Symbols

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Dead Metaphors and Digital Assumptions

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What is Really Intuitive? Mapping the Learnability of Visuals

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Illusion of Intuition: Why “Obvious” Visuals Are Not Always Obvious

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not All Visuals Are Instantly Understood

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Choosing the Right Visuals Across Healthcare Communication

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Rise of Visual Communication in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Flexible Visuals within a Fixed Logic

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not Everyone Reads the Same Picture in the Same Way

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Designing Visuals That Teach And Not Just Tell

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Seeing is not Understanding: Visual Literacy and Why It Matters in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Are Icons Really Universal? Rethinking Visual Language in Global Healthcare

Health Communication
HealthTech
Health Beliefs
From Text to Visual: How Reading Behaviour is Changing in the Digital Age

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Pushing the Round Peg of Typography Through the Square Hole of Culture

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Script Complexity, Typography and COA Design

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: The Hidden Impact of Layout Mismatches on Reading Efficiency

Health Communication
Health Promotion
Patient Voice
Public & Global Health
The Anatomy of Reading: Rethinking Logo Placement in Patient-Facing Materials

Health Communication
Public & Global Health
How Culture Shapes the Way We Read Clinical and Technical Documents

HealthTech
Patient Voice
Health Beliefs
As the Ox Turns: The Biological, Cultural and Technological Limits of Reading

Health Communication
Health Promotion
When Cultural Differences in Information Processing and Typography Create Barriers in COA Localisation

Health Communication
Patient Voice
Linguistic Validation of Clinical Outcome Assessments (COAs): A Checkbox Activity or an Opportunity for Research?

Health Communication
HealthTech
Patient Voice
What does Cognitive Debriefing NOT Cover in a Clinical Outcome Assessment?

Health Communication
Patient Voice
Response Biases and Cognitive Differences in the Cross-Cultural Use of Clinical Outcomes Assessments

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Cultural and Contextual Considerations in the COA Localisation Process

Health Communication
Public & Global Health
Audience Design in Health Communication: Tailoring the Message for Effective Engagement

Health Communication
HealthTech
Formality and Politeness in Clinical Outcome Assessments (COAs) – A Sociolinguistic Perspective on Audience Design

Health Communication
Health Promotion
Patient Voice
Cultural Coating in COA Translation: Overcoming Linguistic and Semantic Barriers

Health Communication
Health Promotion
Health Beliefs
Common Problems of Localisation in Clinical Outcome Assessments (COAs)

Health Communication
Not the Yellow from the Egg: Using Figurative Language in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Taboo Topics in Health: How These Can Lead to ‘Cultural Coating’ of Items in COA Development

Health Communication
Addressing Lexical Ambiguities in Clinical Outcome Assessments: Design with the Entire World in Mind

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Eight tips for Best Practice in Questionnaire Design in Clinical Outcome Assessments

Health Communication
Patient Voice
Public & Global Health
Clinical Outcome Assessments: investing millions only to get the basics wrong?

Health Communication
Patient Voice
Health Beliefs
Assent: Information Overload and Cultural Communication Styles

Health Communication
Patient Voice
Redesigning Assent Forms in International Clinical Research

Health Communication
Patient Voice
A Critique of Clinical Trial Informed Consent and Patient Information Sheets in Clinical Trials

Health Communication
Health Promotion
Patient Voice
Public & Global Health
A Comparison of Formative versus Summative Readability Testing

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Readability User Testing: Strengths, Weaknesses and Strategic Approaches for Patient Information Leaflets

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Essential Tips for Creating IFUs That People Actually Read

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Do not do these 10 mistakes when designing Risk Minimisation Patient Cards

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Clear as Mud: The Hidden Complexity of Simple Drug Instructions

Health Communication
Public & Global Health
Not So Simple: The Hidden Complexity of Everyday Drug Instructions

Health Communication
Public & Global Health
Health Beliefs
Lost in Translation: The Hidden Confusion Behind Simple Medicine Instructions

Health Communication
HealthTech
Public & Global Health
The Opportunities and Challenges of Electronic Patient Information Leaflets (ePILs)

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Knowledge Gap Is Still a Choice

Health Communication
Public & Global Health
Common Design Shortcomings in Written Patient Information

Health Communication
Public & Global Health
Patient Engagement in the form of Patient Information Leaflets. Has the needle even moved since the 2000s?

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Consequences of the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Narrowing the Knowledge Gap between the Pharmaceutical Industry and Their Consumers

Health Communication
Patient Voice
Bridging the Knowledge Gap in Patient Communication in the Provider-Patient Relationship

Health Communication
HealthTech
Patient Voice
Health Beliefs
The Impact of the Knowledge Gap on Patient Well-being

Health Communication
Patient Voice
Face-Sensitive Patient Documentation Across Cultures: Can One Size Fit All?

Health Communication
Patient Voice
Health Beliefs
Face-Sensitive Communication in Pharma: Cultural Impacts on Patient Engagement

Health Communication
HealthTech
Patient Voice
Considerations of ‘Face-Sensitivity’ when Planning Patient-Facing Documentation

Health Communication
Patient Voice
The Blind Spot of Pharma: Information Design as an ‘Unknown Unknown’

Health Communication
Patient Voice
Face Maintenance and Patient Voice in Patient Engagement: The Ideal versus Reality

Health Communication
Patient Voice
Beyond Words: How Face Maintenance Shapes Patient Communication and Engagement

Health Communication
Patient Voice
Can the Pragmatics of Face Maintenance be Mapped onto Patient Engagement Practices?

Patient Voice
Public & Global Health
Health Beliefs
Global Perspectives on Patient Engagement in Clinical Settings

HealthTech
Patient Voice
Patient Engagement in Clinical Practice: what are the key differences between the UK and the USA?

Patient Voice
Health Beliefs
The Cultural Dimensions of Patient Engagement: Challenges for the Pharmaceutical Industry

Health Communication
Patient Voice
Why is Tokenism Rife in the Adoption of Patient Voice Activities?

Health Promotion
Patient Voice
Public & Global Health
The Knowledge Gap between the Medical Establishment and the Patient is a Choice

Patient Voice
Health Beliefs
This Far but No Further: the Cruel Fiction of Patient Empowerment

Health Communication
HealthTech
Patient Voice
The ‘Service Refugee’ Companies Chasing Patient Voice Research: What They Should Know

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Sliding Scale of Sincerity towards the Patient Voice Agenda

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
In Spite of Our Business Model

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Linking Up the Silos

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
A Belated Introduction to Gibson Research Consultancy (GRC)

Patient Voice
Health Beliefs
Challenges of Integrating Patient Voice into Clinical Research in Turkey

Patient Voice
Avoiding Tokenism: Strategies for Meaningful Involvement in Patient and Public Involvement (PPI) Research

Patient Voice
Why Does Tokenistic Patient and Public Involvement (PPI) in Research Occur?

Patient Voice
Understanding Lived Experience Research: A Person-Centred Approach to Knowledge

Patient Voice
The History of Lived Experience Research and Patient and Public Involvement

Patient Voice
Becoming a Lived Experience Researcher – Or, in Layman’s Terms, Putting the Psycho in Psychology
All
Insights
News
Articles
Videos
Search articles…

Health Communication
HealthTech
Patient Voice
Public & Global Health
Cliniphai and Gibson Research Consultancy Partner to Streamline Global COA and eCOA Translation Workflows
Featured
Health Communication
HealthTech
Patient Voice
The Nine Circles of Burden: Real-World Constraints on Patient Memory
Featured

Health Communication
Patient Voice
The Cognitive Burden Simulator: Complex Frequency Item on Distressing Mental Imagery
Health Communication
Patient Voice
The Cognitive Burden Simulator: Checklist, Multi-Select PRO Items
Health Communication
Patient Voice
The Cognitive Burden Simulator: A Frequency Self-Report Item

Health Communication
Patient Voice
The Cognitive Burden Simulator: A Multi-Step Global Evaluation Item (With Follow-Up)

Health Communication
Patient Voice
The Cognitive Burden Simulator: The case of a COA Item with a Binary Response Choice

Health Communication
HealthTech
Patient Voice
From Google to ChatGPT: Offloading, Cognitive Debt and the Future of COAs

Health Communication
Patient Voice
Beyond the Magic: Baddeley’s Working Memory and Multi-Component Strain

Health Communication
Patient Voice
The Nine Circles of Burden: Mapping the Hidden Demands of COAs

Health Communication
Patient Voice
Working Memory and Clinical Outcome Assessments: A Comparative Load Analysis

Health Communication
Patient Voice
Background Behind the Cognitive Burden Simulator: Understanding the Hidden Demands of Clinical Outcome Assessments

Health Communication
Patient Voice
The Cognitive Burden Simulator: Visualising the Hidden Cognitive Burden of Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Cognitive Load and Non-Western Script Readers in Clinical Questionnaires: General Issues
Health Communication
Patient Voice
Cognitive Load and Shared-Stem Questions in Non-Western Script Contexts

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cognitive Load in Translation: Non-Western Patient Experiences with Western COAs

Health Communication
Health Promotion
Cognitive Load in Patient Communication: Patient Information Leaflets and Clinical Outcome Assessments Contrasted

Health Communication
Patient Voice
Reducing Cognitive Load in Clinical Outcome Assessments: Lessons from Mental Health, Pain Management and Oncology

Health Communication
Patient Voice
Cognitive Load in Clinical Outcome Assessments: Optimising Question Design for Better Data Quality
Health Communication
HealthTech
The Google Effect and Miller’s Magic Number: Implications for Questionnaire and Clinical Outcome Assessment Design.

Health Communication
Health Beliefs
Why the Presentation Often Stays the Same from Source to Target

Deep in the Shallow End: The emotional power of sacred trash that was never meant to last.

Health Communication
Patient Voice
The Field Beyond: Rumi, Reductionism and the Texture of Qualitative Knowing

The Conman Chronicles: Fictional Conversations between an AI Agent and a Wannabe New ‘Expert’

Health Communication
Patient Voice
Health Beliefs
Culture and Cognition in Survey Responses in Healthcare

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What I’ve Learnt About Using Visual Metaphors in Explainer Videos

Health Communication
Health Promotion
HealthTech
Public & Global Health
Designing Icons for Crisis, Emergency and Risk Communication

Health Communication
Why Visual Clarity Can Save Lives: Designing for thinking under stress.

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Empowered Patient: A Privileged Identity?

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Cross-Cultural Aspects of the Locus of Control

Patient Voice
Health Beliefs
When Control Lies Beyond: The External Locus of Control in Healthcare and Life

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Power Within: Internal Locus of Control as a Core of Patient Empowerment

Health Communication
Patient Voice
Owning the Outcome: Understanding the Internal Locus of Control in Health and Beyond

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
When the Sublime Offends: Ethical Collisions and Cultural Limits

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Ambiguous States, Ambivalent Roles: Liminality in the Clinical Encounter

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Beyond Beauty: Reclaiming the Sublime in Culture and Care

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Biographical Disruption and the Liminal Self

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
The Threshold of Meaning: The Liminality of Culture in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Measuring What Matters: How Do You Capture Resonance in Health Communication?

Patient Voice
Public & Global Health
Exploring Research Design: The Grand Heist’s Blueprint

Health Communication
Patient Voice
Public & Global Health
Why Does Informed Consent Matter?

Health Communication
Patient Voice
Public & Global Health
5 Tips for Achieving Truly Informed Consent in Research

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Messaging and Culture: Reaching What Lies Beneath

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion Campaigns Fall Flat When They Ignore the Depths

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Charting the Unseen: What COAs Miss Beneath the Cultural Waterline

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Every Individual is a Culture of One. Responding to the Sublime in Healthcare

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Sublime: Culture’s Deep and Unseen Role in Shaping Health Behaviours

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Culture is Never a Frozen List of Traits

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
What Linguistic Relativity Really Looks Like. How language shapes attention, memory and perception across cultures

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 2: Time to Let it Melt

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Fifty Words for Snow. Part 1: Language, Culture and Conceptual Equivalence in Translation

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Health Promotion and Health Beliefs

Health Communication
HealthTech
Patient Voice
Public & Global Health
The Vice of Time and Cost

HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Dragonfly Trapped in Amber: When Method Becomes Dogma

Health Communication
Patient Voice
Public & Global Health
Linguistic Validation Specialisation Course

Health Communication
HealthTech
The Predictable Rhetoric of AI-Generated Text: Overused Stylistic Devices

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
"Sí da / No da": Calm Public Health Messaging That Worked

Health Communication
Health Promotion
Public & Global Health
How Smart Public Health Campaigns Avoid the Irony Trap

Health Communication
Health Promotion
Public & Global Health
The Irony Trap: How public health messages get hijacked by culture

Patient Voice
Public & Global Health
Health Beliefs
Gynecology in Turkey: Navigating Cultural and Social Taboos

Health Communication
Public & Global Health
Health Beliefs
Addressing Mental Health Stigma in Turkey

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Experiments in Language: AI as a Co-Creator in Global Health Communication

Health Communication
HealthTech
Rethinking Work: The Personal and Professional Shift with AI

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Semiotics of the White Coat in Media Communication

Health Communication
Health Promotion
Public & Global Health
Epilogue: The Tylenol-Autism Debate, the Knowledge Gap and the Future of Trust

Health Communication
Health Promotion
Public & Global Health
“Tough It Out”: The Long Dismissal of Women’s Pain

Health Communication
Health Promotion
Public & Global Health
The “Tough It Out” Line: Why It Resonated, Why It Harms

Health Communication
Health Promotion
HealthTech
Public & Global Health
Why Falsehoods Travel Faster: The Facts versus Emotion Gap

Health Communication
Health Promotion
Public & Global Health
Speaking in Facts, Hearing in Feelings

Health Communication
Health Promotion
Public & Global Health
The Tylenol-Autism Controversy: Communication, Power and the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Did We Bend Technology Out of Shape? From the Handaxe to the Health App

Health Communication
HealthTech
What’s That Coming Over the Hill? How We Use AI In Our Work

Health Communication
HealthTech
Public & Global Health
Bridging Concept Elaboration and Translatability in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Translatability in Clinical Outcome Assessments: Designing for the Global Patient Voice

Health Communication
Patient Voice
Health Beliefs
Concept Elaboration in Clinical Outcome Assessments: An intersection of Language, Science and Culture

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Do Not Ignore Visuals When Testing Materials

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Designing Beyond Obsolescence

Health Communication
Health Promotion
HealthTech
Public & Global Health
The Lifecycle of Visual Symbols

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Dead Metaphors and Digital Assumptions

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
What is Really Intuitive? Mapping the Learnability of Visuals

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
The Illusion of Intuition: Why “Obvious” Visuals Are Not Always Obvious

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not All Visuals Are Instantly Understood

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Choosing the Right Visuals Across Healthcare Communication

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
The Rise of Visual Communication in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Flexible Visuals within a Fixed Logic

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Not Everyone Reads the Same Picture in the Same Way

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Designing Visuals That Teach And Not Just Tell

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Seeing is not Understanding: Visual Literacy and Why It Matters in Healthcare

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Are Icons Really Universal? Rethinking Visual Language in Global Healthcare

Health Communication
HealthTech
Health Beliefs
From Text to Visual: How Reading Behaviour is Changing in the Digital Age

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Pushing the Round Peg of Typography Through the Square Hole of Culture

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: Script Complexity, Typography and COA Design

Health Communication
Health Promotion
Public & Global Health
The Anatomy of Reading: The Hidden Impact of Layout Mismatches on Reading Efficiency

Health Communication
Health Promotion
Patient Voice
Public & Global Health
The Anatomy of Reading: Rethinking Logo Placement in Patient-Facing Materials

Health Communication
Public & Global Health
How Culture Shapes the Way We Read Clinical and Technical Documents

HealthTech
Patient Voice
Health Beliefs
As the Ox Turns: The Biological, Cultural and Technological Limits of Reading

Health Communication
Health Promotion
When Cultural Differences in Information Processing and Typography Create Barriers in COA Localisation

Health Communication
Patient Voice
Linguistic Validation of Clinical Outcome Assessments (COAs): A Checkbox Activity or an Opportunity for Research?

Health Communication
HealthTech
Patient Voice
What does Cognitive Debriefing NOT Cover in a Clinical Outcome Assessment?

Health Communication
Patient Voice
Response Biases and Cognitive Differences in the Cross-Cultural Use of Clinical Outcomes Assessments

Health Communication
Patient Voice
Public & Global Health
Health Beliefs
Cultural and Contextual Considerations in the COA Localisation Process

Health Communication
Public & Global Health
Audience Design in Health Communication: Tailoring the Message for Effective Engagement

Health Communication
HealthTech
Formality and Politeness in Clinical Outcome Assessments (COAs) – A Sociolinguistic Perspective on Audience Design

Health Communication
Health Promotion
Patient Voice
Cultural Coating in COA Translation: Overcoming Linguistic and Semantic Barriers

Health Communication
Health Promotion
Health Beliefs
Common Problems of Localisation in Clinical Outcome Assessments (COAs)

Health Communication
Not the Yellow from the Egg: Using Figurative Language in Clinical Outcome Assessments

Health Communication
Patient Voice
Health Beliefs
Taboo Topics in Health: How These Can Lead to ‘Cultural Coating’ of Items in COA Development

Health Communication
Addressing Lexical Ambiguities in Clinical Outcome Assessments: Design with the Entire World in Mind

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
Eight tips for Best Practice in Questionnaire Design in Clinical Outcome Assessments

Health Communication
Patient Voice
Public & Global Health
Clinical Outcome Assessments: investing millions only to get the basics wrong?

Health Communication
Patient Voice
Health Beliefs
Assent: Information Overload and Cultural Communication Styles

Health Communication
Patient Voice
Redesigning Assent Forms in International Clinical Research

Health Communication
Patient Voice
A Critique of Clinical Trial Informed Consent and Patient Information Sheets in Clinical Trials

Health Communication
Health Promotion
Patient Voice
Public & Global Health
A Comparison of Formative versus Summative Readability Testing

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Readability User Testing: Strengths, Weaknesses and Strategic Approaches for Patient Information Leaflets

Health Communication
Health Promotion
HealthTech
Public & Global Health
Health Beliefs
Essential Tips for Creating IFUs That People Actually Read

Health Communication
Health Promotion
Public & Global Health
Health Beliefs
Do not do these 10 mistakes when designing Risk Minimisation Patient Cards

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Clear as Mud: The Hidden Complexity of Simple Drug Instructions

Health Communication
Public & Global Health
Not So Simple: The Hidden Complexity of Everyday Drug Instructions

Health Communication
Public & Global Health
Health Beliefs
Lost in Translation: The Hidden Confusion Behind Simple Medicine Instructions

Health Communication
HealthTech
Public & Global Health
The Opportunities and Challenges of Electronic Patient Information Leaflets (ePILs)

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Knowledge Gap Is Still a Choice

Health Communication
Public & Global Health
Common Design Shortcomings in Written Patient Information

Health Communication
Public & Global Health
Patient Engagement in the form of Patient Information Leaflets. Has the needle even moved since the 2000s?

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Consequences of the Knowledge Gap

Health Communication
HealthTech
Patient Voice
Public & Global Health
Narrowing the Knowledge Gap between the Pharmaceutical Industry and Their Consumers

Health Communication
Patient Voice
Bridging the Knowledge Gap in Patient Communication in the Provider-Patient Relationship

Health Communication
HealthTech
Patient Voice
Health Beliefs
The Impact of the Knowledge Gap on Patient Well-being

Health Communication
Patient Voice
Face-Sensitive Patient Documentation Across Cultures: Can One Size Fit All?

Health Communication
Patient Voice
Health Beliefs
Face-Sensitive Communication in Pharma: Cultural Impacts on Patient Engagement

Health Communication
HealthTech
Patient Voice
Considerations of ‘Face-Sensitivity’ when Planning Patient-Facing Documentation

Health Communication
Patient Voice
The Blind Spot of Pharma: Information Design as an ‘Unknown Unknown’

Health Communication
Patient Voice
Face Maintenance and Patient Voice in Patient Engagement: The Ideal versus Reality

Health Communication
Patient Voice
Beyond Words: How Face Maintenance Shapes Patient Communication and Engagement

Health Communication
Patient Voice
Can the Pragmatics of Face Maintenance be Mapped onto Patient Engagement Practices?

Patient Voice
Public & Global Health
Health Beliefs
Global Perspectives on Patient Engagement in Clinical Settings

HealthTech
Patient Voice
Patient Engagement in Clinical Practice: what are the key differences between the UK and the USA?

Patient Voice
Health Beliefs
The Cultural Dimensions of Patient Engagement: Challenges for the Pharmaceutical Industry

Health Communication
Patient Voice
Why is Tokenism Rife in the Adoption of Patient Voice Activities?

Health Promotion
Patient Voice
Public & Global Health
The Knowledge Gap between the Medical Establishment and the Patient is a Choice

Patient Voice
Health Beliefs
This Far but No Further: the Cruel Fiction of Patient Empowerment

Health Communication
HealthTech
Patient Voice
The ‘Service Refugee’ Companies Chasing Patient Voice Research: What They Should Know

Health Communication
Health Promotion
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
The Sliding Scale of Sincerity towards the Patient Voice Agenda

Health Communication
HealthTech
Patient Voice
Public & Global Health
Health Beliefs
In Spite of Our Business Model

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
Linking Up the Silos

Health Communication
Health Promotion
Patient Voice
Public & Global Health
Health Beliefs
A Belated Introduction to Gibson Research Consultancy (GRC)

Patient Voice
Health Beliefs
Challenges of Integrating Patient Voice into Clinical Research in Turkey

Patient Voice
Avoiding Tokenism: Strategies for Meaningful Involvement in Patient and Public Involvement (PPI) Research

Patient Voice
Why Does Tokenistic Patient and Public Involvement (PPI) in Research Occur?

Patient Voice
Understanding Lived Experience Research: A Person-Centred Approach to Knowledge

Patient Voice
The History of Lived Experience Research and Patient and Public Involvement

Patient Voice